This case is a patient in his 30s who is construction worker (high demand) and was seen in the office due to his R clavicle fracture. He presented to the office with R clavicle pain due to a fracture that was 5 weeks old. He was concerned about his ability to return to work after healing of this fracture in conservative fashion ie treatment in a sling. Xrays demonstrated a displaced clavicle fracture with more than 2 cm of shortening. We elected to proceed with open reduction and internal fixation due to his profession and the radiographic appearance of the fracture. Xrays prior and after the fixation as shown below. In addition, the evidence for surgical approach for this type of injury is reported below (AAOS)
Do all displaced midshaft clavicle fractures need surgery?
By Jennie McKee
Point/counterpoint: ORIF or nonsurgical treatment
Whether an athlete falls off a bicycle, is tackled in a football game, or is slammed into the side of the hockey rink by another player, the result can be the same: a displaced midshaft clavicle fracture. When this potentially season-ending injury occurs, it’s not always clear whether conservative treatment or surgical fixation will yield the best patient outcomes.
Brian H. Mullis, MD, and Edward G. McFarland, MD, explored the pros and cons of both treatment strategies during a point/counterpoint session at the 2011 Specialty Day meeting of the American Orthopaedic Society of Sports Medicine.
Benefits of surgical fixation
According to Dr. Mullis, treating displaced midshaft clavicle fractures with open reduction and internal fixation (ORIF) can offer several benefits compared to conservative treatment, because athletes can get back on the field sooner.
In a prospective, randomized, multicenter study of more than 100 patients with displaced midshaft clavicle fractures, for example, the nonsurgical group healed at an average of 28 weeks, while the surgical group healed at an average of 16 weeks.
“I’m assuming most patients would like the much shorter healing time that surgical fixation provided in that study,” he said, adding that surgery offered other benefits as well.
“Researchers found that patients treated nonsurgically had higher malunion and nonunion rates and worse outcomes,” he said.
Those conclusions were reinforced by another prospective, observational study that also found higher nonunion rates in patients treated nonsurgically.
“The study found a 30 percent nonunion rate and a 36 percent symptomatic malunion rate in the nonsurgical group,” he said, “while the surgical group did much better.” He added that both the Constant and the American Shoulder and Elbow Surgeons (ASES) scores were worse in the nonsurgical group at all time points in the study.
Strength in the affected limb can also be an issue with nonsurgical treatment, he said. Although many patients likely have good long-term results when treated nonsurgically, some studies have found a correlation between nonsurgical treatment and decreased strength.
He noted that a 5-year follow-up study found that patients had a 20 percent to 30 percent loss of strength on the injured side compared to the uninjured side. They also had much worse functional scores on the injured side.
Indications for surgery
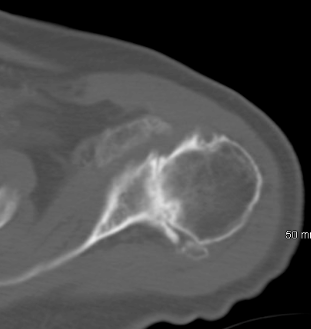
“Absolute indications for surgery include open fractures and neurovascular injury requiring repair or exploration,” said Dr. Mullis, who suggested that the strongest relative indication for surgery is a displaced clavicle with 2 cm or more of shortening (Fig. 1). Other relative indications include multiple extremity involvement, floating shoulder, seizure disorders, and cosmesis.
|
|
|
|
Fig. 1 (From top): Pre- and postoperative radiographs of a patient who underwent surgical fixation of a displaced midshaft clavicle fracture. Courtesy of Brian H. Mullis, MD
|
“I’ll be the first to admit that for an athlete with a truly nondisplaced fracture, the risks of surgery outweigh the benefits,” said Dr. Mullis, “and I certainly would not provide surgical treatment for children, who heal well with nonsurgical treatment. I would also not recommend surgery for patients with low functional demands.”
ORIF is “not without its perils”
Like Dr. Mullis, Dr. McFarland believes that ORIF can be the best treatment option for displaced midshaft clavicle fractures in competitive athletes early in the season, but cautions that not every clavicle fracture needs surgical fixation.
“The question a treating orthopaedist should ask is not, ‘Should I surgically repair this injury in the athlete?’ but ‘Is this the type of fracture I would repair surgically in any patient?’”
Variables such as degree of displacement, shortening, and comminution should be carefully considered. Other variables include location of the injury (dominant or nondominant arm), the patient’s activity level, status of the physes (open or closed), and the existence of other injuries.
“An orthopaedist needs to reconsider the advantages of giving that patient 2 or 3 extra weeks to compete, if, for example, the patient is not making a living from a sport or not involved in sports at all,” he said.
He agreed with Dr. Mullis that children with open physes generally should not undergo surgical fixation.
Surgical complications
“Whenever you do operate on patients with this injury, you have to weigh the benefits and the risks,” said Dr. McFarland. “Incisional numbness and hardware irritation are real and not infrequent complications, as are scar concerns and the risk of infection.”
Studies support the risk of surgical complications. In one study, 53 percent of surgical patients required plate removal. In another study of 125 patients who underwent ORIF, 12 percent needed reoperation, 4 percent had plate breakage, and 3.2 percent had loosening. Other complications included infection and frozen shoulders.
“This tells us that ORIF is not without its perils,” he said. “And the question is, does it really give us that much of an advantage?”
Studies have shown, said Dr. McFarland, that healing time with a clavicle reconstruction plate is 14.6 weeks; healing time with a compression plate is 13 weeks. A study of professional football players found that nonsurgical treatment yielded a healing time of 7 weeks, compared to a healing time of 8.8 weeks with ORIF.
“And, remember, the sooner the patient returns to sport, the greater the risk that another injury might occur,” he added.
Some studies suggest, said Dr. McFarland, that providing conservative treatment and waiting to see if a nonunion occurs, rather than initially treating the patient surgically, may not pose significant risks. He pointed to a study that found that if nonunions are operated on later—meaning, after the patient has undergone conservative treatment and subsequently required surgical fixation for a nonunion—the results are almost the same as with immediate ORIF.
“I tell most of my patients—even those with displaced fractures—not to be concerned about a nonunion, because if it does occur, we will repair it surgically later, and they will be as good as they were before,” he said.
In closing, Dr. McFarland emphasized that treatment should be individualized to the patient and the fracture pattern.
“ORIF in midseason is a viable option in some athletes,” he said, noting that patients must be educated about the possibility of complications and the need for reoperation. Despite these risks, he said, “surgical fixation can be satisfying in the right patient.”
Dr. McFarland acknowledged the assistance of Juan Garzon-Muvdi, MD, in preparing his presentation.
Disclosure information: Dr. Mullis—Synthes, Amgen, AO, Medtronic. Dr. McFarland—Stryker DePuy-Mitke; DePuy, A Johnson & Johnson Company; Stryker; and DJ Orthopaedics; American Journal of Sports Medicine; Journal of Athletic Training; Clinical Orthopaedic and Related Research; Medicine and Science in Exercise and Health.
Jennie McKee is a staff writer for AAOS Now
. She can be reached atmckee@aaos.org
Bottom Line
- When treating displaced midshaft clavicle fractures, orthopaedists must take many variables into account, including (but not limited to) the degree of displacement, shortening, comminution, patient age (open epiphysis), and the existence of other injuries.
- According to some studies, ORIF enables athletes with displaced midshaft clavicle fractures to return to sport sooner than conservative treatment.
- Drawbacks of surgical fixation can include hardware irritation and removal, incisional numbness, infection, and scar concerns.
- Although ORIF can be a valid option in appropriate patients, orthopaedists should ask whether this is the type of fracture that needs an operation in any patient before proceeding.
References:
- Canadian Orthopaedic Trauma Society: Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007;89(1):1-10.
- Kulshrestha V, Roy T, Audige L: Operative versus nonoperativemanagement of displaced midshaft clavicle fractures: A prospective cohort study. J Orthop Trauma 2011;25(1):31-38.
- McKee MD, Pedersen EM, Jones C, et al: Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am 2006;88(1):35-40.
- Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D,Kralinger FS: Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures: A randomized, controlled, clinical trial. J Orthop Trauma2009;23(2):106-112.
- Ferran NA, Hodgson P, Vannet N, Williams R, Evans RO: Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: A randomized clinical trial. J Shoulder Elbow Surg. 2010;19(6):783-789.
- Potter JM, Jones C, Wild LM, Schemitsch EH, McKee MD: Does delay matter? The restoration of objectively measured shoulder strength and patient-oriented outcome after immediate fixation versus delayed reconstruction of displaced midshaft fractures of the clavicle.J Shoulder Elbow Surg 2007;16(5):514-518. Epub Jul 12, 2007.


.JPG)

























