Preoperative images are seen above
First dislocation is seen above 3 weeks after index procedure
Revision to thicker polyethylene provided stability for a short period of time (2 weeks)
At two weeks after the revision to a thicker polyethylene the shoulder was dislocated anteriorly and interestingly the patient
1. was not aware of when or how this happened
2. had NO PAIN.
During the past 7 years of my shoulder practice I have used the reverse TSA to solve complex problems of failed prior shoulder operations and never had a dislocation. I am not sure I understand the exact reason of this failure. An attempt is made below to identify the cause.
Identifiable reasons for dislocations are:
1. Male gender
2. Infection
3. Non compliance with restrictions in activity
4. Trauma
5. Prior shoulder surgery with an unstable prior arthroplasty - greatest risk
6. Soft tissue imbalance
7. Implant design
8. Scapular notching
9. Subscapularis release and choice of no repair back to humerus
10. Impingement to bony structures or soft tissue
11. High BMI
12. Component malpositioning
13. Abutment of the medial aspect of the humeral cup against the scapular neck causing the humeral component lever away from glenosphere.
14. Loose soft tissue tensioning.
From those factors only number 1, 3, 7 can be considered in this case as the revision surgery and evaluation of the shoulder intra-operatively eliminated the other factors.
In the Australian registry 2016 (Data Period 1 September 1999 – 31 December 2015) the proportion of rTSA has increased from 43.7% in 2010 to 64.1% in 2015. In the same registry the majority of revisions of reverse total shoulder replacements were done for dislocation or instability. However, it is not mentioned how many of those remained stable. In general the rate of revision after rTSA is 3-10% for instability or dislocation and it is the most common complication in the majority of published series of rTSA. In the Australian registry instability or dislocation accounts for 38% of all revisions.
Some implant designs are prone to high chances of impingement as seen below, as the humerus or polyethylene is in close proximity with the glenoid.
Bottomline is we are still learning about the reverse total shoulder prosthesis and there is a lot of space for improvement in the design and patient selection process.
While initially the patient elected to avoid a 3rd operation, later on during the course of his treatment he decided to proceed with conversion to a hemi-arthoplasty. Pictures below show that his scapula is superiorly tilted. This scapula position, is different compared to superior glenoid wear which is seen in rotator cuff arthropathy. Correction of this scapula alignment with over-reaming inferiorly could have been a possible solution, however the eccentric glenoid reaming and removal of glenoid bone inferiorly would be have extensive and thus weakening the fixation and of glenosphere to the glenoid .
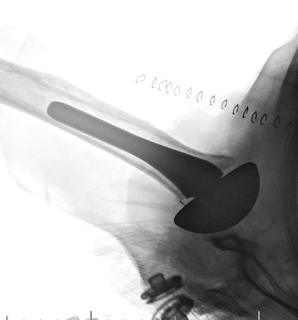
The films after the conversion to hemi-arthroplasty are seen below: