Most of time the type C glenoid represents a combination of posterior humeral de-centering, with bone deficiency of the glenoid posteriorly as well as posterior erosion and retroversion of the glenoid surface. Exposure and reaming of the glenoid can be very difficult as insertion of a reamer requires further posterior translation of the humerus.
Correction of the retroversion with resection of anterior glenoid bone is not recommended as this requires significant bone removal, reaming pass the subchondral plate and exposure of cancellous bone which does not provide good fixation for a glenoid implant. In addition, such bone resection will eventually decrease the size of the glenoid and lead to smaller glenoid -socket- which increases instability.
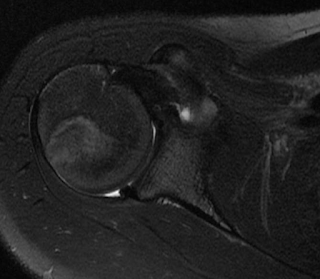
Below is a case of primary osteoarthritis of the shoulder with significant retroversion and a type C glenoid. The retroversion was to 60 degrees which was addressed with concentric reaming of the glenoid and implantation of an anterior eccentric head, as well as, closure of the rotator cuff interval.
The AP xray above demonstrates the medial erosion of the glenoid as shown by the acromial index. The method of calculation of the acromion index is shown below.
The axillary x-ray was not "a true" axillary view as the spinoglenoid notch cannot be seen. For this reason a CT was obtained which gives better understanding of the glenoid deformity.
There was 60 degrees of retroversion of the glenoid while the humeral head was posteriorly subluxated. As shown below the ration of AB/AC should be approximately 50% in order for the humeral head to "sit" in the center of the glenoid. In our case this ratio was 0%.
The AB/AC ratio was increased with placement of an anteriorly directed eccentric head. The humeral cut was "conservative" to avoid "under-stuffing of the joint and instability. The drop-back during passive forward elevation was addressed with soft tissue balancing by closure of the rotator cuff interval
As seen on this last x-ray, hypothetical implantation of a glenoid component would have placed the construct in high risk of early glenoid failure due to posterior edge loading of the glenoid implant. For this reason a hemi-arthroplasty was performed with concentric reaming of the glenoid.
Six months after surgery she has significant improvement in active forward elevation with near full active forward elevation.
Simulation of her postoperative motion is shown below