(1) Degree of the glenoid deformity. Correction or no correction of the deformity?
*(2) Reaming to subchondral or pass the subchondral plate? It seems that the implanted glenoid component is mostly supported by the subchondral bone
(3) Sizing of the implant. Larger or smaller implant?
(4) Use of step cut glenoid component or not
(5) Penetration of the glenoid vault or not?
In the case example provided below a preoperative CT scan demonstrates no glenoid deformity and implantation of a anchored pegged glenoid component was performed without penetration of the glenoid vault. It seems that pressurization of the cement in intact glenoid vault would be ideal if there is no cortex penetration. Although it is critical when keeled glenoid components are used it seems that it has no implications when anchored pegged glenoid components are used. The reason is that we do not use cement for the central peg. In case of penetration it seems that for the central anchored ingrowth peg there will be "bicortical fixation".
Further reading:
Edge displacement and deformation of glenoid components in response to eccentric loading. The effect of preparation of the glenoid bone. D Collins, A Tencer, J Sidles and F Matsen. J Bone Joint Surg Am. 1992;74:501-507
 |
| Central anchored peg contained in the glenoid vault |
 |
| Grashey view shows the height of the prosthesis and alignment |
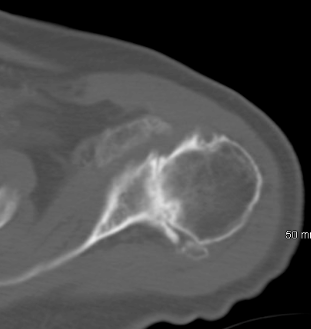 |
| Preoperative CT scan shows no glenoid deformity. |
.JPG)










